| Tell me when this page is updated |
| Tell me when this page is updated |
 Get the Genesis
of Eden AV-CD by secure internet order
>> CLICK_HERE
Get the Genesis
of Eden AV-CD by secure internet order
>> CLICK_HERE
Windows / Mac Compatible. Includes live video
seminars, enchanting renewal songs and a thousand page illustrated
codex.
 Return to Genesis of Eden?
Return to Genesis of Eden?
Germ Warfare A drug-resistant staph strain has doctors on edge New Scientist 97
Staphylococcus aureus, Mycobacterium
tuberculosis, Escherischia coli
all have antibiotic-resistant strains which
can become untreatable (Scientific American Mar 98 32)
OF ALL THE ILLNESSES THAT CAN BE picked up in the hospital, a staphylococcus infection is surely the most fearsome. The stealthy bacterium snakes along intravenous lines or seeps into surgical wounds, destroying skin and bones, poisoning blood, threatening death. For years it could be stopped by penicillin. Then it slowly became resistant to one antibiotic after another until finally only one, vancomycin, remained to subdue all staph strains. Now comes word that even that microbial barrier is falling. Last week the Centers for Disease Control reported that a man in a Michigan hospital had contracted a staph infection that even vancomycin could not stem. It was just the second report of a vancomycin-resistant staph infection. The first case occurred in japan last year when a baby became ill after heart surgery. By using several antibiotics simultaneously, the doctors in Michigan brought their patient's infection under control. Even so, health officials suspect that vancomycin-resistant staph will soon appear in other U.S. hospitals as well. Calling for stringent antiseptic procedures, they urged doctors to report cases of vancomycin-resistant staph promptly to the CDC. Bacteria, of course, don't become resistant on their ovm. Whenever antibiotics are used indiscriminately, mildly resistant bacteria survive and breed with one another, creating increasingly resistant germs. Pharmaceutical companies are racing to create new antibiotics that can replace vancomycin as the drug of last recourse. The leading candidate: Synercid, an experimental drug being developed by Rhone Poulene Rorer. Tests show that it should defeat even vancomycin-resistant staphylococci-at least until a tougher strain of bacteria evolves. - By Christine Gorman

"Don't forget to take a handful
of our complimentary antibiotics on your way out"
New Yorker Jan 12 98
34
Researchers from France and Madagascar report in the latest New England Journal of Medicine that they have found a strain of bubonic plague resistant to most ofthe antibiotics used to treat and prevent the disease that savaged Europe in the Middle Ages.

Superbugs take hold New Scientist 25 Apr 98 4
THE routine use on farms of drugs that are related to human antibiotics should be banned, says the House of Lords Select Committee on Science and Technology. In a report issued this week, the committee adds that the agency that monitors the "alarming" spread of drug-resistant bacteria is being starved of funds. The Lords' warnings are given weight by news of the emergence of another antibiotic-resistant "superbug". New Scientist has learnt that the Public Health Laboratory Service (PHLS) has identified a new multidrug-resistant bacterium, which could kill people with weak immune systems. Many farmers routinely feed antibiotics to animals such as pigs and chickens because this can increase their growth by up to five per cent. But some of these antibiotics are related to important human drugs, and scientists fear that the drug resistance in farmyard bacteria produced by this indiscriminate dosing with antibiotics will spread to human pathogens. The Lords' report says that a ban on the use of growth promoters belonging to the same class as human drugs should be introduced, "preferably bv voluntary agreement ... but by legislation if necessary". Veterinary drug companies sav that there is scant evidence of resistance being transferred from farms, but committee chairman Lord Soulsby argues that the threat posed by bacteria that can infect vulnerable hospital patients means that a safety-first approach is essential. "Humans are the most important consideration," he says. "It's possible methicillin- resistant Staphylococcus aureiis will become untreatable" (see Figure). Officials at the Ministry of Agriculture, Fisheries and Food accept that pressure to ban growth promoters is likely to grow. "Our view is that, in the long term, the use of such chemotherapeutics will need to be minimised, if not stopped," says David Shannon, the ministry's chief scientist. The Lords committee's report also criti- cises recent cuts in the Department of Health's funding of the PHLS. This has fallen by 12 per cent over the past three years, and the department's plans predict further reductions. "It is astonishing that funding for the PHLS is falling at a time when the surveillance of infectious disease and particularly resistant disease has become so important," says Soulsbv Diana Walford, director of the PHLS, says that the agency is developing a com- prehensive programme for the surveillance of drug resistance, relying on routine reporting from hospitals rather than look- ing only at bacterial samples sent to the PHLS for analvsis. But its success will depend on more money, she savs- "We're going to have to have additional funds if we're going to do the job properly." The PHLS's current efforts to monitor the emergence of drug-resistant bacteria are spearheaded by its Antibiotic Reference Unit. David Livermore, who directs the unit, says his team has found a strain of Pseudomonas aeruginosa resistant to "just about everything", including the current antibiotics of last resort, carbapenems- "This gives a worrying indication of how resistance is on the rise in a broad range of pathogens," he says. P. aertiginosa causes a wide range of infections in people who are ill or have damaged immune systems, including lung infections in people with cystic fibrosis and septicaemia in patients receiving treatment for leukaemia. Drug resistance is a growing problem in treating these infections, says Stephen Barrett of St Mary's Hospital in London. "We usually manage to find some older, obscure drugs that work, but maybe we've just been lucky so far." Michael Day
Less is More New Scientist 25 Apr 98 3
IT IS not often that the conclusions of an important report are prefaced by the words: "This inquiry has been an alarming experience . . . ", especially when those responsible are the members of the House of Lords Select Committee on Science and Technology. But these peers-who include many renowned scientists and doctors among their number-have every reason to be alarmed. They have confronted the dreadful prospect that resistance to antibiotics is spreading widely, that some poorer parts of the world have already been plunged back into the era before anti- biotics, and that early next century there may come a time when resistant bacteria appear faster than the drugs to treat them. Some degree of resistance is inevitable. But, as the report explains, the West has made the spread of resistance worse through careless overprescribing by doctors, perhaps by the use of antibiotics to speed the growth of farm animals, and in Britain, by cuts in the National Health Ser- vice that have helped some hospitals become reservoirs of antibiotic-resistant bacteria. This news will not surprise many scien- tists who have been invited to conference after conference on the subject over the past few years. But it will be a profound shock for a public that takes antibiotics so completely for granted that they cannot imagine what life would be like without them. Perhaps they should ask those who can remember the 1920s. Then, tuberculosis meant isolation in a sanatorium until you died or cured yourself, simple hospital op- erations could mean death by infection, cuts and scratches might result in fatal septi- caemia and syphilis often ended in insanity. If we want to keep antibiotics effective, national and global action will be necessary. First, we must accept that there are good rea- sons for reducing the use of antibiotics to a minimum. The inquiry heard that doctors often prescribe antibiotics because patients ask for them and that explaining why it might be better not to use them just takes too much time. Doctors themselves have often been too long out of college to fully under- stand the risks of the spread of resistance. The cures are obvious: media campaigns, posters in every doctor's waiting room and re-education courses for doctors themselves. Secondly, the use of antibiotics in farm animals needs to be controlled much more tightly. At the very least, animals and humans should not be given related antibiotics (see p 4). But in the longer term, the regular use of antibiotics as "growth promoters" will probably have to end, as it already has in Sweden. The evidence that resistance has spread from anin-als to humans is limited. But there is a terrifying possibility that bac- teria in animals being fed antibiotics could evolve some very general resistance iechanism, such as the ability to pump antibiotic out of them- selves. Resistance to whole classes of antibiotics might thus appear, spread to humans and wipe out established disease treatments. Thirdly, hospitals in Britain and elsewhere need to relearn old hygiene skills and reduce dependence on antibiotics. Con- ditions described in the report would make Florence Nightingale turn in her grave. Cost-cutting in Britain means that hos- pitals are not properly cleaned, beds are too close together, and "hot bedding"-where patients move around the hospital as beds become free-spreads infections every- where. Isolation wards have vanished to save money and basic standards, such as washing hands between patients, have slipped. With an educated public and tighter con- trol of usage, could antibiotic resistance be not just controlled but reduced? Optimists suggest when a bacterium acquires genes to provide resistance it does so at a cost, so that resistant bacteria would once again be replaced by non-resistant ones if the use of a particular antibiotic was stopped. That would mean we could stay ahead of disease by carefully revolving the use of different antibiotics. Unfortunately, the latest evidence suggests that some bacteria can simply acquire other mutations that allow them to keep resistance at little cost. If that is generally true, then the future looks grim. Some bits of the world are already experiencing the horrors that result when drugs fail. In Tadzhikistan, a strain of typhoid fever has emerged that is resistant to every known antibiotic. One drugs company told the inquiry that between 2000 and 2007, multi-resistant organisms will emerge "without parallel progress in the introduction of new antibiotic classes". We have been warned.
The Challenge of Antibiotic Resistance Stuart Levy Scientific American Mar 98 12
Last year an event doctors had been fearing finally occurred. In three geographically separate patients, an often deadly bacterium, Staphylococcus aureus, responded poorly to a once reliable antidote-the antibiotic vancomycin. Fortunately, in those patients, the staph microbe remained susceptible to other drugs and was eradicated. But the appearance of S. aureus not readily cleared by vancomycin foreshadows trouble. Worldwide, many strains of S. aureus are already resistant to all antibiotics except vancomycin. Emergence of forms lacking sensitivity to vancomycin signifies that variants untreatable by every known antibiotic are on their way. S. aureus, a major cause of hospital-acquired infections, has thus moved one step closer to becoming an unstoppable killer. The looming threat of incurable S. aureus is just the latest twist in an international public health nightmare: increasing bacterial resistance to many antibiotics that once cured bacterial diseases readily. Ever since antibiotics became widely available in the 1940s, they have been hailed as miracle drugsmagic bullets able to eliminate bacteria without doing much harm to the cells of treated individuals. Yet with each passing decade, bacteria that defy not only single but multiple antibiotics-and therefore are extremely difficult to control-have become increasingly common. What is more, strains of at least three bacterial species capable of causing lifethreatening illnesses (Enterococcus faecalis, Mycobacterium tuberculosis and Pseudomonas aerliginosa) already evade every antibiotic in the clinician's armamentarium, a stockpile of more than 100 drugs. In part because of the rise in resistance to antibiotics, the death rates for some communicable diseases (such as tuberculosis) have started to rise again, after having declined in the industrial nations. How did we end up in this worrisome, and worsening, situation? Several interacting processes are at fault. Analyses of them point to a number of actions that could help reverse the trend, if individuals, businesses and governments around the world can find the will to implement them. One component of the solution is recognizing that bacteria are a natural, and needed, part of life. Bacteria, which are microscopic, single-cell entities, abound on inanimate surfaces and on parts of the body that make contact with the outer world, including the skin, the mucous membranes and the lining of the intestinal tract. Most live blamelessly. In fact, they often protect us from disease, because they compete with, and thus limit the proliferation of, pathogenic bacteria-the minority of species that can multiply aggressively (into the millions) and damage tissues or otherwise cause illness. The benign competitors can be important allies in the fight against antibiotic-resistant pathogens. People should also realize that although antibiotics are needed to control bacterial infections, they can have broad, undesirable effects on microbial ecology. That is, they can produce long-lasting change in the kinds and proportions of bacteria-and the mix of antibiotic-resistant and antibiotic-susceptible typesnot only in the treated individual but also in the environment and society at large. The compounds should thus be used only when they are truly needed, and they should not be administered for viral infections, over which they have no power.
A bad combination
Though many factors can influence whether bacteria in a person or in a community will become insensitive to an antibiotic, the two main forces are the prevalence of resistance genes (which give rise to proteins that shield bacteria from an antibiotic's effects) and the extent of antibiotic use. If the collective bacterial flora in a community have no genes conferring resistance to a given antibiotic, the antibiotic will successfully eliminate infection caused by any of the bacterial species in the collection. On the other hand, if the flora possess resistance genes and the community uses the drug persistently, bacteria able to defy eradication by the compound will emerge and multiply. Antibiotic-resistant pathogens are not more virulent than susceptible ones: the same numbers of resistant and susceptible bacterial cells are required to produce disease. But the resistant forms are harder to destroy. Those that are slightly insensitive to an antibiotic can often be eliminated by using more of the drug; those that are highly resistant require other therapies. To understand how resistance genes enable bacteria to survive an attack by an antibiotic, it helps to know exactly what antibiotics are and how they harm bacteria. Strictly speaking, the compounds are defined as natural substances (made by living organisms) that inhibit the growth, or proliferation, of bacteria or kill them directly. In practice, though, most commercial antibiotics have been chemically altered in the laboratory to improve their potency of to increase the range of species they affect. Here I will also use the term to encompass completely synthetic medicines, such as quinolones and sulfonamides, which technically fit under the broader rubric of antimicrobials. Whatever their monikers, antibiotics, by inhibiting bacterial growth, give a host's ii-nmuile defenses a chance to outflank the bugs that remain. The drugs typically retard bacterial proliferation by entering the niicrobes and interfering with the production of coniponelits needed to form new bacterial cells. For instance, the antibiotic tetracycline hinds to ribosomes (internal structures that make new proteins) and, in so doing, impairs protein manufacture; penicillin and vancomycin impede propcr synthesis of the bacterial cell wall. Certain resistance genes ward off destruction by giving rise to enzymes which degrade antibiotics or that chemically modify, and so inactivate, the drugs. Alternatively, some resistance genes cause bacteria to alter or replace molecules that are normally bound by an antibiotic changes that essentially eliminate the drug's targets in bacterial cells. Bacteria might also eliminate entry ports for the drugs or, more effectively, may manufacture pumps that export antibiotics before the medicines have a chance to find their intracellular targets.
My Resistance Is Your Resistance
Bacteria can acquire resistance genes through a few routes. Many inherit the genes from their forerunners. Other times, genetic mutations, which occur readily in bacteria, will spontaneously produce a new resistance trait or will strengthen an existing one. And frequently, bacteria will gain a defense against an antibiotic by taking up resistance genes from other bacterial cells in the vicinity. Indeed, the exchange of genes is so pervasive that the entire bacterial world can be thought of as one huge multicellular organism in which the cells interchange their genes with ease. Bacteria have evolved several ways to share their resistance traits with one another [see "Bacterial Gene Swapping in Nature," by Robert V. Miller; Scientific American, January]. Resistance genes commonly are carried on plasmids, tiny loops of DNA that can help bacteria survive various hazards in the environment. But the genes may also occur on the bacterial chromosome, the larger DNA molecule that stores the genes needed for the reproduction and routine maintenance of a bacterial cell. Often one bacterium will pass resistance traits to others by giving them a useful plasmid. Resistance genes can also be transferred by viruses that occasionally extract a gene from one bacterial cell and inject it into a different one. In addition, after a bacterium dies and releases its contents into the environment, another will occasionally take up a liberated gene for itself. In the last two situations, the gene will survive and provide protection from an antibiotic only if integrated stably into a plasmid or chromosome. Such integration occurs frequently, though, because resistance genes are often embedded in small units of DNA, called transposons, that readily hop into other DNA molecules. In a regrettable twist of fate for human beings, many bacteria play host to specialized transposons, termed integrons, that are like flypaper in their propensity for capturing new genes. These integrons can consist of several different resistance genes, which are passed to other bacteria as whole regiments of antibiotic-defying guerrillas. Many bacteria possessed resistance genes even before commercial antibiotics came into use. Scientists do not know exactly why these genes evolved and were maintained. A logical argument holds that natural antibiotics were initially elaborated as the result of chance genetic mutations. Then those which turned out to eliminate competitors, enabled the manufacturers to survive and proliferate-if they were also lucky enough to possess genes that protected them from their own chemical weapons. Later, these protective genes found their way into other species, some of which were pathogenic. Regardless of how bacteria acquire resistance genes today, commercial antibiotics can select for-promote the survival and propagation of-antibiotic-resistant strains. In other words, by encouraging the growth of resistant pathogens, an antibiotic can actually contribute to its own undoing.
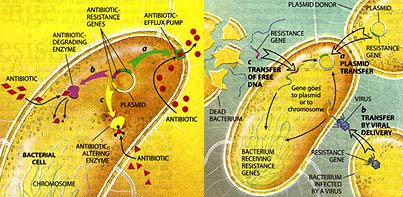
BACTERIA PICK UP
RESISTANCE GENES from other bacterial cells in three main ways. Often they
receive whole plasmids bearing one or more such genes from a donor cell (a).
Other times, a virus wdi pick up a resis- tance gene from one bacterium and
inject it into a different bacterial ceu (b). Alternatively, bacteria sometimes
scavenge gene-bearing snippets of DNA from dead cells in their vicinity (c).
Genes obtained through viruses or from dead cells persist in their new owner if
they become incorporated stably into the recipient's chromosome or into a
plasmid.
How Antibiotics Promote Resistance
The selection process is fairly straightforward. When an antibiotic attacks a group of bacteria, cells that are highly susceptible to the medicine will die. But cells that have some resistance from the start, or that acquire it later (through mutation or gene exchange), may survive, especially if too little drug is given to overwhelm the cells that are present. Those cells, facing reduced competition from susceptible bacteria, will then go on to proliferate. When confronted with an antibiotic, the most resistant cells in a group will inevitably outcompete all others. Proniotiiig resistance in known pathogens is nor the only self-defe.iting of antihi,)tics. When the medicines attack disease-causing bacteria, they also affect benign bacteria innocent bystanders-in their path. They eliminate drug-susceptible bystanders that could otherwise limit the expansion of pathogens, and they simultaneously encourage the growth of resistant bystanders. Propagation of these resistant, nonpathogenic bacteria increases the reservoir of resistance traits in the bacterial population as a whole and raises the odds that such traits will spread to pathogens. in addition, sometimes the growing populations of bystanders themselves become agents of disease. Widespread use of cephalosporin antibiotics, for example, has promoted the proliferation of the once benign intestinal bacterium E. faecalis, which is naturally resistant to those drugs. In most people, the immune system is able to check the growth of even multidrugresistant E. faecalis, so that it does not produce illness. But in hospitalized patients with compromised immunity, the enterococcus can spread to the heart valves and other organs and establish deadly systemic disease. Moreover, administration of vancomycin over the years has turned E. faecalis into a dangerous reservoir of vancomycin-resistance traits. Recall that some strains of the pathogen are multidrug-resistant and are responsive only to vancomycin. Because vancomycin-resistant E. faecalis has become quite common, public health experts fear that it will soon deliver strong vancomycin resistance to those S. aureus strains, making them incurable. The bystander effect has also enabled multidrug-resistant strains of Acinetobacter and Xantbomonas to emerge and become agents of potentially-fatal blood borne infections in hospitalized patients. These formerly innocuous microbes were virtually unheard of just five years ago. As I noted earlier, antibiotics affect the mix of resistant and nonresistant bacteria both in the individual being treated and in the environment. When resistant balteria arise in treated individuals, these microbes, like other bacteria, spread readily to the surrounds and to new hosts. Investigators have shown that when one member of a household chronically takes an antibiotic to treat acne, the concentration of antibiotic-resistant bacteria in family members rises. Similarly, heavy use of antibiotics in such settings as hospitals, day care centers and farms (where the drugs are often given to livestock for nownedicinal purposes) increases the levels of resistant bacteria in people and other organisms who are not being treated - including in individuals who live near the epicenters of high consumption or who pass through the centers. Given that antibiotics and other antimicrobials, such as fungicides, affect the kinds of bacteria in the environment and people around the individual being treated, I often refer to these substances societal drugs-the only class of therapeutics that can be so designated. Anticancer drugs, in contrast, affect only the person taking the medicines. On a larger scale, antibiotic resistance that emerges in one place can often spread far and wide. The ever increasing volume of international travel has hastened transfer to the U.S. of multidrugresistant tuberculosis from other countries. And investigators have documented the migration of a strain of multidrug-resistant Streptococcus pneiimoniae from Spain to the U.K., the U.S., South Africa and elsewhere. This bacterium, also known as the pneumococcus, is a cause of pneumonia and meningitis, among other diseases.

Spread of resistant Streptococcus
pneumonae
illustrates rapid global dissemination of resistant strains
Antibiotic Use Is Out of Control
To those who understand that antibiotic delivery selects for resistance, it is not surprising that the intemational community currently faces a major public health crisis. Antibiotic use (and misuse) has soared since the first commercial versions were introduced and now includes many nonmedicinal applications. In 1954 two million pounds were produced in the U.S.; today the figure exceeds 50 million pounds. Human treatment accounts for roughly half the antibiotics consumed every year in the U.S. Perhaps only half that use is appropriate, meant to cure bacterial infections and administered correctly-in ways that do not strongly encourage resistance. Notably, many physicians acquiesce to misguided patients who demand antibiotics to treat colds and other viral infections that cannot be cured by the drugs. Researchers at the Centers for Disease Control and Prevention have estimated that some 50 million of the 150 million outpatient prescriptions for antibiotics every year are unneeded. At a seminar I conducted, more than 80 percent of the physicians present admitted to having written antibiotic prescriptions on demand against their better judgment. In the industrial world, most antibiotics are available only by prescription, but this restriction does not ensure proper use. People often fail to finish the full course of treatment. Patients then stockpile the leftover doses and medicate themselves, or their family and friends, in less than therapeutic amounts. in both circumstances, the improper dosing will fail to eliminate the disease agent completely and will, furthermore, encourage growth of the most resistant strains, which may later produce hard-totreat disorders. In the developing world, antibiotic use is even less controlled. Many of the same drugs marketed in the industrial nations are a,.,ailable over the counter. Unfortunately, when resistance becomes a clinical problem, those countries, which often do not have access to expensive drugs, may have no substitutes available. The same drugs prescribed for human therapy are widely exploited in animal husbandry and agriculture. More than 40 percent of the antibiotics manufactured in the U.S. are given to animals. Some of that amount goes to treating or preventing infection, but the lion's share is mixed into feed to promote growth. In this last application, amounts too small to combat infection are delivered for weeks or months at a time. No one is entirely sure how the drugs support growth. Clearly, though, this long-term exposure to low doses is the perfect formula for selecting increasing numbers of resistant bacteria in the treated animals-which mav then pass the microbes to caretakers and, more broadly, to people who prepare and consume undercooked meat. In agriculture, antibiotics are applied as aerosols to acres of fruit trees, for controlling or preventing bacterial infections. High concentrations may kill all the bacteria on the trees at the time of spraying, but lingering antibiotic residues can encourage the growth of resistant bacteria that later colonize the fruit during processing and shipping. The aerosols also hit more than the targeted trees. They can be carried considerable distances to other trees and food plants, where they are too dilute t(, eliminate full-blown infections but are still capable of killing off sensitive bacencourage growth of the most resistant strains, which may later produce hard-totreat disorders. In the developing world, antibiotic use is even less controlled. Many of the same drugs marketed in the industrial nations are available over the counter. Unfortunately, when resistance becomes a clinical problem, those countries, which often do not have access to expensive drugs, may have no substitutes available. The same drugs prescribed for human therapy are widely exploited in animal husbandry and agriculture. More than 40 percent of the antibiotics manufactured in the U.S. are given to animals. Some of that amount goes to treating or preventing infection, but the lion's share is mixed into feed to promote growth. In this last application, amounts too small to combat infection are delivered for weeks or months at a time. No one is entirely sure how the drugs support growth. Clearly, though, this long-term exposure to low doses is the perfect formula for selecting increasing numbers of resistant bacteria in the treated animals-which mav then pass the microbes to caretakers'and, more broadly, to people who prepare and consume undercooked meat. In agriculture, antibiotics are applied as aerosols to acres of fruit trees, for controlling or preventing bacterial infections. High concentrations may kill all the bacteria on the trees at the time of spraying, hut lingering antibiotic residues can encourage the growth of resistant bacteria that later colonize the fruit during processing and shipping. The aerosols also hit more than the targeted trees. They can be carried considerable distances to other trees and food plants, where they are too dilute to eliminate full-blown infections but are still capable of killing off sensitive hacteria and thus giving the edge to resistant versions. Here, again, resistant bacteria can make their way into eople through the food chain, finding a p home in the intestinal tract after the produce is eaten, The amount of resistant bacteria people acquire from food apparently is not trivial. Denis E. Corpet of the National Institute for Agricultural Research in Toulouse, France, showed that when human volunteers went on a diet consisting only of bacteria-free foods, the number of resistant bacteria in their feces decreased 1,000-fold. This finding suggests that we deliver a supply of resistant strains to our intestinal tract whenever we eat raw or undercooked items. These bacteria usually are not harmful, but thev could be if by chance a disease-causing type contaminated the food. T'he extensive worldwide exploitation of antibiotics in medicine, animal care and agriculture constantly selects for strains of bacteria that are resistant to the drugs. Must all antibiotic use he halted to stem the rise of intractable bacteria? Certainiv not. But if the drugs are to retain their power over pathogens, they have to be used more responsibly. Society can accept some increase in the fraction of resistant bacteria when a disease needs to he treated; the rise is unacceptable when antibiotic use is not essential.
Reversing Resistance
Number of corrective measures can be taken right now. As a start, farmers should be helped to find inexpensive alternatives for encouraging an imal growth and protect-ng fruit trees. Improved hygiene, for instance, could go a lorig way to ciihaiicing livestock development. The puhlic can wash raw fruit and vegetables thoroughly to clear off both resistant bacteria and possible antibiotic residues. When they receive prescriptions for antibiotics, they should complete the full course of therapy (to ensure that all the pathogenic baicteria die) and should not "save" any pills for later use. (consumers also should refrain from demanding antibiotics for Colds and other viral infections and might consider seeking nonantibiotic therapies for niinor conditions, such as certain cases of acne. Thev can continue to put antibiotic ointments oii small cuts, but they should think twice about routinely using hand lotions and a proliferation of other products now imbued with antibacterial agents. New laboratory findings indicate that certain of the bacteria-fighting chemicals being incorporated into consumer products can select for bacteria resistant both to the antibaterial preparations and to antibiotic drugs. Physicians, for their part, can take some immediate steps to minimize any resistance ensuing from required uses of antibiotics. When possible, they should " to identify the causative pathogen before beginning therapy, so they can prescribe an antibiotic targeted specificallv to that microbe instead of having to choose a broad-spectrum product. Washing hands after seeing each patient is a major and obvious, but too often overlooked, precaution. To avoid spreading multidrug-resistanc infections between hospitalized patients, hospitals place the affected patients iii separate rooms, where they are seen by gloved and gowned health workers and visitors. This practice should continue. Having new antibiotics could provide tnore options for treatment. In the 1980s pharmaceutical manufacturers, thinking infectious diseases were essentially conquered, cut back severely on searching for additional antibiotics. At the time, if one drug failed, another in the arsenal would usually work (at least in the industrial nations, where supplies are plentiful). Now that this happy state of affairs is coming to an end, researchers are searching for novel antibiotics again. Regrettably, though, few drugs are likely to pass soon all technical and regulat tory hurdles needed to reach the market. Furthermore, those that are close to being ready are structurally similar to existing antibiotics; they could easily encounter bacteria that already have defenses against them. With such concerns in mind, scientists are also working on strategies that will give new life to existing antibiotics. Many bacteria evade penicillin and its relatives by switching on an enzyme, penicillinase, that degrades those compounds. An antidote already on pharmacy shelves contains an inhibitor of penicillinase; it prevents the breakdown of penicillin and so frees the antibiotic to work normally. In one of the strategies under study, my laboratory at Tufts University is developing a compound to jam a microbial pump that ejects tetracycline from bacteria; with the pump inactivated, tetracycline can penetrate bacterial cells effectively.
Considering the Environmental Impact
As exciting as the pharmaceutical research is, overall reversal of the bacterial resistance problem will require public health officials, physicians, farmers and others to think about the effects of antibiotics in new ways. Each time an antibiotic is delivered, the fraction of resistant bacteria in the treated individual and, potentially, in others, increases. These resistant strains endure for some time-often for weeks-after the drug is removed. The main way resistant strains disappear is by squaring off with susceptible versions that persist in-or enter-a treated person after antibiotic use has stopped. In the absence of antibiotics, susceptible strains have a slight survival advantage, because the resistant bacteria have to divert some of their valuable energy from reproduction to maintaining antibiotic-fighting traits. Ultimately, the susceptible microbes will win out, if they are available in the first place and are not hit by more of the drug before they can prevail. Correcting a resistance problem, then, requires both improved management of antibiotic use and restoration of the environmental bacteria susceptible to these drugs. If all reservoirs of susceptible bacteria were eliminated, resistant forms would face no competition for survival and would persist indefinitely. In the ideal world, public health officials would know the extent of antibiotic resistance in both the infectious and benign bacteria in a community. To treat a specific pathogen, physicians would favor an antibiotic most likely to encounter little resistance from any bacteria in the community. And they would deliver enough antibiotic to clear the in-faction completelv but would not rop long therapy so much as to destroy all susceptible bystanders in the body. Prescribers would also take into account the number of other individuals in the setting who are being treated with the same antibiotic. If many patients in a hospital ward were being given a particular antibiotic, this high density of use would strongly select for bacterial strains unsubmissive to that drug and would eliminate susceptible strains. The ecological effect on the ward would be broader than if the total amount of the antibiotic were divided among just a few people. If physicians considered the effects beyond their individual patients, thev might decide to prescribe different anti 'biotics for different patients, or in different wards, thereby minimizing the selective force for resistance to a single medication. Put another way, prescribers and public health officials might envision an 'antibiotic threshold": a level of antibiotic usage able to correct the infections within a hospital or community but still falling below a threshold level that would strongly encourage propagation of resistant strains or would eliminate large numbers of competing, susceptible microbes. Keeping treatment levels below the threshold would ensure that the original microbial flora in a person or a community could be restored rapidly by susceptible bacteria in the vicinity after treatment ceased. The problem, of course, is that no one yet knows how to determine where that threshold lies, and most hospitals and communities lack detailed data on the nature of their microbial populations. Yet with some dedicated work, researchers should be able to obtain both kinds of information. Control of antibiotic resistance on a wider, international scale will require cooperation among countries around the globe and concerted efforts to educate the world's populations about drug resistance and the impact of improper antibiotic use. As a step in this direction, various groups are now attempting to track the emergence of resistant bacterial strains. For example, an intemational organization, the Alliance for the Prudent Use of Antibiotics (P.O. Box 1372, Boston, MA 02117), has been monitoring the worldwide emergence of such strains since 1981. The group shares information with members in more than 90 countries. It also produces educational brochures for the public and for health professionals. The time has come for global society to accept bacteria as normal, generally beneficial components of the world and not try to eliminate them-except when they give rise to disease. Reversal of resistance requires a new awareness of the broad consequences of antibiotic usea perspective that concerns itself not only with curing bacterial disease at the moment but also with preserving microbial communities in the long run, so that bacteria susceptible to antibiotics will always be there to outcompete resistant strains. Similar enlightenment should influence the use of drugs to combat parasites, fungi and viruses. Now that consumption of those medicines has begun to rise dramatically, troubling resistance to these other microorganisms has begun to climb as well.
Vetrinary Antibiotic Resistance
To illustrate how silly the situation is Hoffmann-La Roche has been producing a vetrinary antiobiotic avoparcin which is closely similar to and acts in the same way as vancomycin and teichoplanin the last drugs available (now gone) capable of treating methicillin resistant staphlococcus aureus MRSA. This is routinely injected into farm animals such as pigs. The first resistance to avoparcin in aminals was already noted in 1987. The spread of avoparcin resistance to MRSA would probably knock out the two human antibiotics as well and could spread from gut coli to staph. New Scientist 27th July 96 7 and 21/28 Dec 96 6 outline the proposal to finally ban this antibiotic.
A Smoking Gun Antibiotic resistance and farming.
New Scientist 21 Mar 98
FARMERS are the prime suspects in the creation of a human 'superbug", according to genetic evidence linking a farmyard antibiotic to the emergence of a drug-resistant human pathogen. The discovery will fuel calls for a ban on the use of antibiotics to promote the growth of farm animals. Bacteria called enterococci normally live harmlessly in the guts of people and animals, but can kill people with impaired immune systems. Increasingly, they are becoming resistant to drugs. And in 1986, a strain that was resistant to vancomycin, an antibiotic used as a last resort, appeared in France. Similar superbugs soon emerged elsewhere in Europe, and from 1989 they spread through hospitals in the US. At first, experts blamed the emergence of vancomycin-resistant enterococci (VRE) on the overuse of antibiotics in hospitals, but studies showing that pigs and poultry harboured VRE ralwd suspicions that perhaps they were originally foodbome pathogens. Animals grow up to five per ceilt faster if they are given antibiotics in their feed. One farmyard antibiotic, avoparcin, is structurally similar to vancomycin-which might explain why some enterococci from farm animals resist vancomycin. Evidence linking human VRE to farmyard antibiotics has been hard to find. But at the emerging diseases meeting, Henrik Wegener of the Danish Veterinary Laboratory in Copenhagen revealed the best data yet. Wegener has sequenced the gene responsible for vancomycin resistance in animal and human enterococci. Aside from the mutation that confers resistance, genes from some of the bacteria also carry a second mutation, where one letter of the genetic code, a G, is replaced with a T. VRE samples from people contained both variants, bacteria from poultry in several countries were all of the T variant, while bacteria from pigs were all G. "This supports the idea that animals are the source of VRE in humans, whereas humans are an unlikely source of VRE for animals," says Wegener. "If that was the case, we would expect to see both in animals." However, Tony Mudd of Roche Products, which makes avoparcin, remains unconvinced: "These are interesting data, but I'm not sure you can categorically state from them that it's one-way traffic of resistance." In 1997, the European Union banned avoparcin, but the general problem remains. For many years in the US and Europe, farmers have fed animals a product called virginiamycin. This resembles Synercid, a new drug to treat VRE. Studies have already revealed Synercid-resistant Enterococcusfaecium in farm animals. "The story about avoparcin and vancomycm is rewriting itself," says Wegener. 'And the drug that was expected to be next in line after Synercid, a compound called Ziracin, is practically identical to a growth promoter called avilamycin, which has been primarily used for poultry.' Again, animal VREs that are resistant to avilamycin are also unaffected by Ziracin. 'Antimicrobial use in food production is a growing threat to human health," agrees David Heymann of the WHO's Division of Emerging and Other Communicable Diseases in Geneva. Wegener believes countries need to get rid of growth promoters enfirely. He says that Sweden did so in 1986 and still produces competitively priced food.' Wegener's concerns are echoed by Britain's National Consumer Council, which last week released a report calling for a Europe-wide ban on the use of antibiotics as growth promoters.
Europe Pushes to Ban Farm Antibiotic New Scientist 21/28 Dec 96
FEARS of an epidemic of deadly "superbugs" have prompted the European Commission to propose a Europe-wide ban on a drug routinely given to farm animals. In a shock move last week, the Commission i recommended that avoparcin, an antibiotic, should be taken off the market. The European Union's member states will decide whether to back the proposal this week. For more than three decades, European fanners have fed avoparcin to livestock to keep them healthy so that they grow faster. But Denmark and Germany banned the drug last year, claiming that if resistance to avoparcin developed in the farmyard, it might spread to bacteria in hospitals. This could make the bacteria resistant to a related antibiotic called vancomycin, which is the last line of defence against killers such as methicillinresistant Staphylococcus aureus. Some governments saw the Danish and German bans as a barrier to free trade. And in endorsing the Danish and German fears,, t the European Commission has overridden its own panel of experts: the Scientific Committee on Animal Nutrition (SCAN), which advised against a ban in July (This Week, 27 July, p 7). The Swiss-based multinational Hoffmann-La Roche, which makes avoparcin, is furious that the Commission has overruled its own scientific advisers. "We think it's a very -hasty measure," says Neil Stafford, Roche's marketing manager for Europe. "All the science says avoparcin doesn't transfer resistance." But the Commission denies it is ignoring science. 'Our proposal is based on scientific opinion," says a spokesman. "The committee couldn't conclude that there would not be transmission from animal to human antibiotics." Some microbiologists applaud the Commission's caution. 'I think it's great news," says Julian Davis of the University of British Columbia in Vancouver. The final decision now rests with representatives from the EU's member states. Besides Germany and Denmark, Finland and Sweden are expected to support the Commission's proposal. But other EU members were not revealing their stance in advance of this week's meeting. Andy Coghlan
New Scientist 27 July 96
EUROPE is embroiled in a battle between free trade and human health. The row centres on avoparcin, an antibiotic which farmers inject into their livestock. Denmark and Germany have recently banned the product because they are worried anitbiotic resistance could spread froni the farmyard into hospitals. Doctors fear they may be left with nothing to treat an antibiotic-resistant 'superbug" sweeping hospitals across the globe. This week a panel of vets that provides independent ad ice to agriculture officials in Bvrussels inflamed the row by rejecting the scientific arguments advanced by Germany and Denmark to justify their action. The conclusion by the European Union's Scientific Committee on Animal Nutrition (SCAN) will make the year-long ban in Denmark and the six-month ban in Germany illegal, on the grounds that they are unfair barriers to trade. Avoparcin, manufactured by the Swiss-based multi-national Hoffmann la Roche, is in the firing line because of its close similarity to antibiotics called vancomycin and teicoplanin. These are the only drugs available that kill methicillin resistant Staphylococclis aureus (MRSA), which is beginning to turn up in hospitals with alarming regularity. Avoparcin. on sale in Europe since 1974, belongs to the same family of antibiotics as vancomycin and teicoplanin and works in exactly the same way. If bacteria in animals become resistant to avoparcin, as was reported for the first time in 1987, the trait s could spread to MRSA in hospitals via faeces, water and food. If MRSA is resistant to avoparcin it will outwit vancomycin and teicoplanin too. And if other species of human gut bacteria - or enterococci become resistant to vancomycin, the crucial genes might 'jump" into MRSA. Germany and Denniark had submitted scientific studies to the SCAN suggesting the threat was real enough to warrant a ban on avoparcin. "We can't quantify the risk, but as a precaution we should not use it any longer," says Wolfgang Witte at the Robert Koch Institute in wernigerode. Witte plesented his results at an international conference on antibiotic-resistant bacteria in London last week, organised by the Ciba Foundation. He has identified vancomycin-. resistant Enterococcus faecium in farm animals and meat products. No resistant enterococci were found in samples from organic farms where antibiotics were not used. The Danish study uncovered three cases of vancomycin-resistant enterococci from hospital patients - although none was actually causing disease. Microbiologists attending last week's conference were dismayed that the SCAN had not upheld the bans. "Farmers should not use any antibiotics that are related to the ones used in humans or that work in the same way," said Julian Davies of the University of British Columbia in Vancouver. Tony Mudd, the technical manager for animal health at Roche roducts, which sells avoparcin in Britain, ays he is delighted with the SCAN's decision, but admits the company is concerned the possibility of resistance spreading m farms to MRSA. "If indepetident data merge that say there's a link and a probem, that product would be off the market in seconds," he says.
Farm animals given antibiotics need less food to grow. Is this use of
drugs destroying a key weapon against human disease? John Bonner
investigates
New Scientist 18 Jan 97
(see also Animal antibiotics threaten hospital epidemics New Scientist 27 July 96 p7)
"THIS little piggy went to market, This little piggy stayed at home..." More likely than not, the little piggy that stayed at home had not reached a marketable size. For nearly fifty years, farmers have been adding low doses of antibiotics to their livestock's food because this improves their feeding efficiency so the animals need less food to reach marketable weight. But now, there is heated debate over whether these additives pose a real risk to human health. Some medical microbiologists want to ban antibiotics from being used as growth promoters on the grounds that they encourage the development of antibiotic-resistant bacteria which could threaten human health. But most scientists who have studied growth promoters and their links to antibiotic resistance in humans say that there is no evidence that they are causing problems. They argue that banning antibiotic growth promoters could increase risks to human health and put poultry, pigs and cattle at risk of disease and death. And on the farms, many are reluctant to forgo the benefits of using antibiotic growth promoters without compelling evidence for a ban. Although there are commercial, economic and ethical aspects to the debate, these need to be carefully separated from scientific assessments of evidence for real risk. Growth-promoting antibiotics are believed to work in animals by controlling low-level diseases which divert energy the animals would otherwise spend putting on weight (See "How antibiotics work", p 26). But the concern is that they could also promote the emergence of bacterial strains which have genetic resistance to antibiotics. As genetic material can be transferred between bacteria, there is every reason to suspect that any genes carrying resistance to antibiotics could also be transferred. Since bacteria with resistance genes would have an obvious advantage over bacteria that succumbed to antibiotics, intense selective pressure would cause resistance to spread throughout bacterial populations. Antibiotic-resistant bacteria could then cause diseases in humans that would be untreatable with conventional antibiotics. In theory, diseases could be contracted directly if animal bacteria get into human food, as happens with food poisoning caused by Salmonella, Campylobacter and Escherichia Coli. But most livestock bacteria can't survive in humans and so are not a threat. Diseases could also be contracted indirectly by the transfer of resistant genes from animal to human bacterial strains. But so far, no natural transfers have been clearly demonstrated. Since the 1960s, public health officials and scientists worldwide have tried to quantify the risks of resistance arising from antibiotic growth promoters, and frame appropriate resFe ponses. The first attempt was the 1969 report of the Swann Committee to the British Parliament. Its recommendation-to prevent antibiotics used in human medicine being given as animal growth promoters-was incorporated into British law. A directive from the European Commission requiring similar restrictions to be enacted by the governments of European Community states was agreed in 1970. In 1986, Sweden considered the issue and decided to ban all antibiotic growth promoters. This decision is one reason why growth promoters have hit the news again recently. When Sweden he EU in 1995, it was to keep its ban, but was until the end of 1998 to r convince the rest of the tates to join its ban, or to drop the ban and fall into line with the other members. The other reason why growth promoters are a hot topic again is controversy over a veterinaty antibiotic called avoparcin, which is closely related to an important medical antibiotic called vancomycin. Denmark and Germany banned avoparcin early last year. (Australia followed suit a few months later.) But then, last summer, the EU's Scientific Committee on Animal Nutrition rejected the scientific basis for the ban (This Week, 27 July 1996, p7). Last month this tale took an unexpected turn when the European Commission chose to ignore the SCAN's advice and called for avoparcin to be banned right across the EU.
Compelling evidence
Other investigations, such as those by the US Office of Technology Assessment in 1979 and the US National Academy of Sciences in the 1980s did not find compelling evidence that fears over antibiotic growth promoters have been realised. The US still allows antibiotics such as penicillin and chlortetracycline to be given as growth promoters even though they are routinely used to treat humans. Victor Lorian, head of the department of epidemiology and infection control at the Bronx-Lebanon Hospital in New York, rejects claims that giving animals low levels of antibiotics compromises human health. Over fifty years in the US, there has been only one compelling case of resistance in a bacterial strain that infects livestock causing disease in humans. That was in 1983 and involved an outbreak of food poisoning caused by a strain of Salmonella that was resistant to a number of antibiotics. The strain was linked to hamburgers made from cattle fed on low doses of chlortetracyline. But even in this case, the evidence was contested: many of the affected people had been dosing themselves with antibiotics which could also have promoted resistance, and because all the cattle had been slaughtered by the time health officials tracked down the source of the outbreak, the resistant Salmonella could only be traced to a neighbouring farm, not to the herd in question. "Considering the millions, if not billions of cattle fed with antibiotics and eaten by man it is clear that the one case is not statistically significant and certainly does not justify banning antibiotics from the food of meat animals," says Lorian. Yet, in Britain, Laura Piddock of the department of infection at the University of Birmingham believes that the American case and a few other cases of possible transmission justify her suspicions that there is a link between resistance in animals and people. She admits that "evidence showing beyond doubt that antibiotic-resistant bacteria arising in animals cause subsequent infection in man which is difficult to treat is difficult to find". She adds that, "only for Salmonella has a natural pathway of transfer of antibiotic resistant bacteria-from animals to foodstuffs to man and subsequent infectionbeen clearly recorded." But even allowing this slender evidence of transmission, it looks as though-at least in Europe-growth promoters cannot be blamed for Salmonella resistance. The growth promoters used in Europe only work against a particular class of bacteria, known as Gram-positive bacteria. Salmonella strains belong to a different class the Gram-negative bacteria. According to David Taylor, a microbiologist at Glasgow veterinary school, "none of the currently registered growth promoters has any effect on Salmonella-any argument for a ban based on the risk of inducing resistance is entirely spurious". Although growth -E promoters affecting Gramnegative bacteria have been used in the US and Australia. there is no substantial evidence of an increase in resistance among Salmonella strains. Instead, Taylor blames the high doses of veterinary antibiotics used to treat infections in livestock for the resistant Salmonella and Campylobacter that are being found in increasing numbers of food poisoning cases in humans. Antibiotics at these concentrations-up to a hundred times those used for growth promotion-kill normal bacteria. And this means that they operate, in evolutionary terms, as a strong selective force on resistant bacteria. Piddock cites the example of a fluoroquinolone antibiotic called enrofloxacin, which vets use in Europe. There is growing evidence, she says, that enrofloxacin is selecting for strains of Campylobacter in poultry that can enter the food chain, and which are resistant to a medical fluoroquinolone called ciprofloxacin.
Gene shuffling
Salmonella (and Campylobacter) are among the few bacteria that can survive in both animal and human hosts. For the majority of strains that cannot, the key issue is whether resistant strains that are specific to animals can transfer their resistance genes to strains that infect humans. There is no clear evidence of natural transfer, but under lab conditions Bill Noble and his colleagues at St Thomas's Hospital, London, reported transferring resistance to the antibiotic vancomycin from Enterococcus faecalis to Staphylococcus aureus. E. faecalis can be transferred to humans in meat products and has been found in human faecal samples. According to Noble, the data show that "it is feasible for resistance genes to transfer between different bacterial strains, but it doesn't show it will happen. It could occur next week, or in 2020, but there are other situations where resistance has not transferred when it could have done." The complex issues of transfer of resistance and risks of cross-resistance to antibiotics have been most widely discussed in debates over avoparcin. This commonly used growth promoter is known to confer cross-resistance to related glycopeptides, including vancomycin. In recent years, vancomycin has become a "last resort" antibiotic in humans, used to treat serious infections caused by the "superbug", methicillin resistant S. aureus (MRSA). Cases of this resistant bacterium are now being reported from increasing numbers of hospitals worldwide. Increases in MRSA are probably due to the heavy use of antibiotics in hospitals and ease of transmission between patients. But the possibility of farmyard resistance to avoparcin eventually promoting resistance to vancomycin in hospitals has been seized on by opponents of growth promoters. Initial research by Frank Aarestrup of the Danish Veterinary Laboratory found evidence of widespread glycopeptide resistance on farms where avoparcin was used and was heavily relied on in justification for the Danish and German bans. In July 1996, the EU's SCAN considered the scientific foundation for the German and Danish bans. its members wanted hard evidence for a natural and sustainable transfer of resistance from livestock to humans, but did not get it. Their report said that Aarestrup had obtained contradictory results in later studies-and that, in any event, he found only small numbers of resistant bacteria which were unable to grow without assistance. The members of SCAN also weighed other evidence for and against the risk of transmission, although it did not publish details of the studies involved. They concluded that early research which had suggested vancomycin resistance could be transferred between bacterial species was contradicted by later, more sensitive studies showing that the genes responsible for vancomycin resistance in human E. faecalis were different from those conferring resistance in strains isolated from pigs and poultry. The SCAN report notes that "it is customary in science to require proof of the positive", and this may be why it recom mended monitoring the avoparcin situation and holding a further review within two years. The recent recommendation by the European Commission to ban avoparcin is apparently also based on "scientific opinion" (This Week, 21/28 December 1996, p 6). But so far, details of any fur ther positive evidence of a risk has not been forthcoming from the Commission. "Blaming animal use of antibiotics is a soft option," says Steve McOrist of the Edinburgh Veterinary School. "Medics should be looking at the infection control procedures in hospitals that allow the spread of resistant strains between patients." The American experience supports his stance: although avoparcin has never been used as a growth promoter in the US, vancomycinresistant bacteria are reported from 15 per cent of American intensive care units. Richard Lacey, a microbiologist at Chapel Allerton Hospital, Leeds, and an outspoken critic of the agricultural industry, says he is also not convinced that using antibiotics as growth promoters is a risk to human health. "I am not bothered about agents which are chemically different from those used in human medicine-there is virtually no possibility of them being a major factor in human disease." But he is strongly opposed to growth promoters and what he regards as other artificial inputs to farming on ethical grounds. others are also worried about the complex ethical and animal welfare dimensions to the arguments. If Europe decides to side with Sweden and impose a ban on all growth promoters, the immediate costs would fall on farm livestock in increased death and disease. McOrist says that in the year following the Swedish ban, an extra 50 000 pigs died of "scours"-or diarrhoea. Whether we like it or not, the health of many farm animals now depends on low doses of antibiotics. Taylor feels that banning the remaining growth promoters used in Europe "will cause problems in the treatment and management of disease which will lead to animals suffering". There are also economic and consumer considerations. Any ban on growth promoters will be at a cost. In late 1995, a report for the European Commission by researchers at the universities of London and Munich estimated that if growth promoters were banned throughout the EU, reduced efficiency and higher treatment costs would increase food costs by 1 billion Ecus (jE750 million) a year.
Trade war
This would inevitably be passed on to the consumers. The report also included a survey of housewives in France, Germany and Britain. Although this found that more than 60 per cent opposed the routine use of antibiotic growth promoters while fewer than 20 per cent actually approved, there is no evidence that these opinions would translate into a ready acceptance of higher prices. A further, less easily measured cost would be the potential for provoking a trade war with other countries that still allow the use of antibiotic growth promoters. This could result in a repeat of problems caused in 1987 when the European Commission banned growth hormones and the US and other countries found they could no longer export meat to Europe. Similar rumblings emerged last year before the Commission's controversial decision, last month, to approve imports of genetically modified maize from the US. Herbert Lundstrbm of the Swedish Veterinary Association still maintains that 11 all unnecessary use of antibiotics -use that is not to prevent or cure disease-should be stopped in the interests of both animals and consumers". He says that Sweden will fight to keep its ban on antibiotic growth promoters. Yet Swedish farmers now have to control many diseases previously kept in check by growth promoters by other methods, including increased reliance on higher doses of therapeutic antibiotics. Their use of tetracyclines doubled between 1988 and 1994. In an ironic twist, it is even possible that a ban on antibiotic growth promoters might inflame the situation that it is supposed to calm.
How antibiotics work
FARMERS have given their livestock antibiotic growth promoters since the 1940s, when their effects were discovered by accident. Scientists were feeding chickens vitamin B12, produced by fermenting bacteria, and found that the birds grew faster than expected. They then realised that the bacteria also produced the antibiotic chlortetracycline. Farmers began using it and other antibiotics to improve weight gain in their animals, reducing the amount of food needed to bring them to market. Exactly how antibiotics enhance performance has never been properly explained. But evidence is now accumulating to show they work by knocking out low-level infections. Therapeutic or preventative doses of antibiotics kill bacteria. By contrast, antibiotics given as growth promoters seem to work at levels which don't affect the ability of beneficial gut bacteria to grow and reproduce but can stunt growth of disease-causing bacteria or tone down the damage they do. In 1995, Lilian Ishida and colleagues from Tohoku University medical school in Japan showed that low doses of antibiotics stop bacteria sticking to cell surfaces in the host, blocking an essential first step in the infection process. Around that time, Mario Jacques of the University of Montreal found that low doses of the antibiotics tylosin and apramycin in livestock prevent bacteria from absorbing the iron needed for growth and reduce the amount of toxic chemicals they release into the host. Tylosin and apramycin are both used as therapeutics, but tylosin is also used as a growth promoter. Victor Lorian of the Bronx-Lebanon Hospital in New York reported that, under laboratory conditions, a number of low-dose antibiotics improve the ability of human and animal white blood cells to recognise and destroy bacteria. Research on how growth promoters work promises a tantalising new angle on the debate over their use. If low-dose antibiotics disable bacteria in different ways from higher, therapeutic doses, it seems likely that the two regimens will also generate different selective pressures for developing resistance.
John Bonner is a freelance science writer based in London.